How is the rhythm of heart contractions maintained?
Aretha
***
Aretha, such a wonderful question!
The heart’s rhythm is so important to life. The heart has four chambers which pump blood along two completely different pathways, and they need to work together. If the different chambers pump out of unison (called dysrhythmia), then they won’t be effective and the person who owns the heart will suffer and maybe die.
First, it is important to understand that the rhythm of the heart is only one measure of heart function. There’s also the heart rate (the number of beats per minute), the stroke volume (how much blood is pumped out with each beat), the preload (how much blood is the body is dumping into the heart before the beat) and the afterload (how much pressure the heart pumps against). All of these work together to make what we call blood pressure.
We can math it up like this:
Stroke Volume = Preload + Rhythm
and
Cardiac Output = Stroke Volume x Heart Rate
and
Blood Pressure = Cardiac Output x Afterload
The rhythm and the rate are the two fundamental building blocks of heart function. And there are two main ways that the heart controls its rate and rhythm: an electrical system and a biofeedback system.
The Electric System
Every single heart muscle cell can, in theory, act as its own pacemaker, but this is not what usually happens. Typically the heart relies on a natural electrical pacemaker system for both rate and rhythm.
The electrical pacemaker system of the heart is amazing. You have three different sets of special cells, called nodes, near the center of your heart. They’re connected to each other by special nerves, and work in tandem to ensure that your heart beats every day of your life!
-
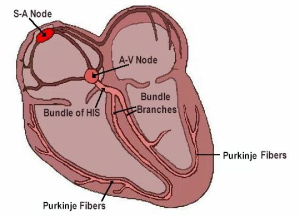
Photo credit: James Eldridge
The SINO-ATRIAL (SA) node sits in the top two chambers of the heart, towards the right. This is the premier pacemaker, and typically beats 60-100 times per minute. It’s the premier because it starts the impulse, and it’s responsible for making sure the top two chambers contract together.
- The ATRIAL-VENTRICULAR (AV) node sits at the junction between the upper and the lower half of the heart. Its primary function is to slow down the impulses coming from the SA node before sending them onward. But if the SA node fails, the AV node can also act as a backup pacemaker. It’s a little slower, though, at 40-60 beats per minute.
- The BUNDLE OF HIS/PURKINJE FIBERS (also known collectively as the ventricular pacemakers) is a collection of nerve fibers that spread out below the AV node and wrap themselves around the lower (and largest) part of the heart. Its job is to spread the impulse from above throughout the bottom two chambers so they contract in unison.
Each pacemaker is listening to the one above it. The AV node will only start firing if it is isolated from the SA node or if the SA node is firing too slow. This might happen in a heart attack, when the tissue surrounding the SA node dies and the SA node no longer functions. The AV node will start firing, taking over the pacemaking function and sending impulses downstream. Redundancy systems inside our own organs – cool, right?
And if both the SA node and the AV node stop sending off electric impulses, the Purkinje fibers will fire all by itself. This is a last-ditch way to keep blood moving, albeit at a much slower rate.
It’s rare, but one way the system can screw up is if the lower pacemakers send impulses back up the heart, the wrong way. Sometimes those special nerve clusters can accidentally catch some of the tissue above them. This is called retrograde condition, but it is uncommon. Don’t even think about the possibility of your heart pumping backwards. Seriously. Quit worrying.
An EKG (electrocardiogram) strip (like on those beep-beep-beep machines you see in every hospital drama) is a representation of the electrical function of the heart. But it’s possible for the electrical system to work, but the heart muscle to not respond to the impulses. In other words, it is indeed possible for a patient to have a normal looking EKG strip, but be clinically dead. This is called Pulseless Electrical Activity (PEA). But don’t worry about that either. It’s fine. You’re fine.
But what about the other mechanism, the biofeedback?
This one is way more complicated. Paramedics spend many many hours trying to learn and understand the very basics of this intricate biochemical interaction. I’ll keep it brief here, though.
Understand: your body likes BALANCE. Moderation in all things. Neither too fast, or too slow. We don’t want too much oxygen (that’d be hyperoxia) or too little (hypoxia). Blood pressure should be neither too high (hypertension) nor too low (hypotension). Body temperature, salt content, carbon dioxide, just about everything in the body exists in balance. And all the little balances come together into one big full-body balance called homeostasis.
But that doesn’t mean that everything is exactly in the middle all the time. Homeostasis fluctuates depending on the needs of the body. Your heart rate speeds up when you’re running, and slows down when you’re sleeping. Mostly, the electrical system keeps your heart inside the homeostasis parameters. It’s only when something dramatic happens that your biofeedback system shows up to push it outside the normal limits.
The body lets your heart know if it needs to kick into high gear through a combination of the autonomic nervous system (which is electricity again) and the endocrine system (your hormones). The main reasons your body might want your heart to speed up are known as the 4 F’s: Fight, Fright, Flight, and Sex… insert your own F-word there.

Pictured: A Problem (photo credit: LadyOfHats)
If you are walking along and a bear jumps out at you, your brain will immediately recognize that this is Not Normal and also A Problem. The brain does two things: directly stimulate the heart by sending an extra zap through the nervous system, and indirectly stimulate the heart by sending out a wave of the hormone adrenaline.* The adrenaline alerts the SA Node about the whole “bear” situation, and tells it to up the heart rate so your heart will pump faster and your body will have more blood to use to run away faster! It also increases your stroke volume and afterload, keeping everything dynamic.
Later, after you get away, as you relax and tell your friends that you definitely had everything under control the whole time and at no point desperately needed another pair of pants, the brain will undo its earlier actions, sending an equal-but-opposite counter-zap through the nervous system and letting the adrenaline fade away. The heart rate returns to normal, restoring homeostasis.
I hope this explanation helps.
Thank you,
The Paramedics Nerd
*In American medical texts adrenaline is usually called “epinephrine.” For some reason.
Got a paramedics question? Ask the Paramedics Nerd! asktheleagueofnerds@gmail.com
Twitter @AskTheLeague / facebook.com/asktheleagueofnerds
References:
Cardiovascular System I: Heart. (n.d.). Retrieved January 7, 2016, from http://www.rci.rutgers.edu/~uzwiak/AnatPhys/Cardiovascular_System.html
VanMeter, K., & Hubert, R. (2014). Cardiovascular System Disorders. In Gould’s pathophysiology for the health professions (Fifth ed). Elsevier.